- Solutions
- Solutions
- Home Health
- Hospice
- Life Plan Community
- Palliative Care
- Private Duty
- Senior Living
- Skilled Nursing
- Skilled Nursing
- Skilled Nursing Software
- Advanced Insights
- Customer relationship management
- Data and analytics
- Financial & operations management
- Marketing
- Nutrition management
- Referral management
- Regulatory compliance
- Retail management
- Resident engagement
- Revenue cycle management
- Skilled nursing interoperability
- Partners
- Blogs
- Resources
- About
- User Conference

The impact of HHCAHPS on VBP: Measures and scoring explained
According to new CMS guidelines, Home Health CAHPS (HHCAHPS) results will factor into 30% of the overall Medicare reimbursement you receive. This means that HHCAHPS survey responses, and how you address the issues and pain points identified in survey results, are a major factor in how you get paid for the care you provide.
What are the HHVBP measures and how are scores calculated? In this blog, we dive into these processes and how home health organizations can maximize their results.
HHVBP is determined by 12 measures
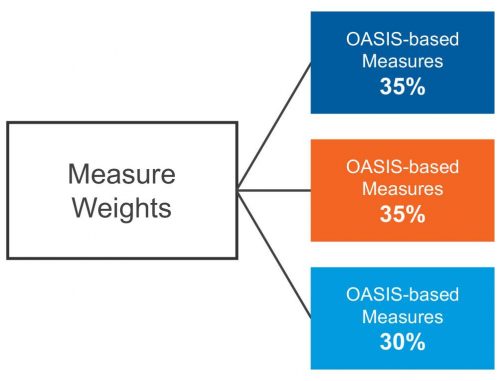
For Home Health Value-Based Purchasing (HHVBP), there are 12 measures pulled from three different data sources: OASIS, claims, and HHCAHPS. Measure calculations for each data source have different minimum volume requirements and weighting and are adjusted for value-based purchasing based on different patient characteristics.
5 OASIS Measures (minimum: 20 quality episodes)
- Improvement in dyspnea
- Discharge to community
- Improvement in oral medication management
- Total Normalized Change (TNC) in self-care
- TNC in mobility
2 Claims Measures (minimum: 20 patient stays)
- Acute Care Hospitalization (ACH) – first 60 days
- Emergency Department (ED) use – first 60 days
5 HHCAHPS Measures (minimum: 40 complete surveys; patients answered at least 50% of questions applicable to all respondents)
- Care of patients
- Communication between providers and patients
- Specific care issues
- Rating of patient care provided by the agency
- Willingness to recommend the agency
HHVBP is determined by 3 scores
From a scoring perspective, achievement and improvement points are calculated by CMS by comparing your agency’s performance score with three different CMS-calculated comparisons:
- Benchmark score: Based on the model baseline year
This score is measure- and cohort-specific and represents the mean of the top 10% of scores. - Achievement threshold: Based on the model baseline year
This score is measure- and cohort-specific and represents the median performance score from the model baseline year. - Improvement threshold: Based on your HHA baseline year
This is your HHA’s performance score from your HHA baseline year.
Cohort groups are defined by the number of unique beneficiaries in the prior calendar year. Smaller-volume cohorts have less than 60 unique beneficiaries and larger-volume cohorts have 60 or more unique beneficiaries.
HHVBP points determine reimbursement
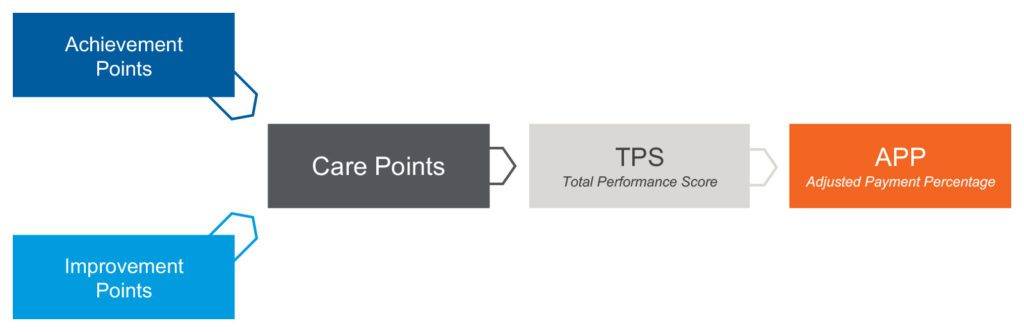
Achievement and improvement threshold points get converted into care points based on whichever one has the highest value. In the example chart below, you see the care points column representing the higher figure.
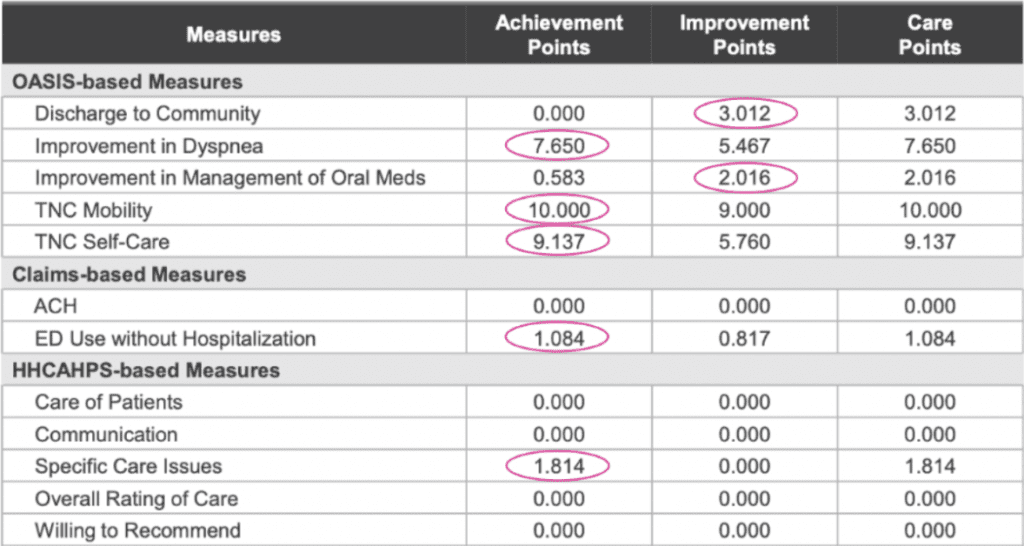
Care points then influence the total performance score and ultimately your APP, which is the adjusted payment percentage — the determining factor for how the reimbursements for your Medicare claims will be increased, decreased or remain the same as the previous year.
The methodology of total performance scoring
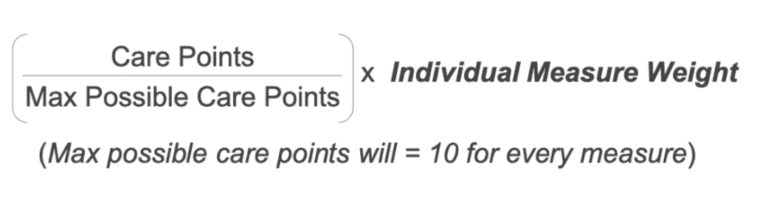
To calculate your Total Performance Score (TPS), first multiply the individual measure weight by the care points that are assigned for each measure, divided by the total maximum number of care points. Each measure is going to have the same maximum possible care points — it will always be a 10, because that is the maximum number for the achievement points.
The care points that you earned divided by 10, multiplied by that measure weight is going to give you your weighted measure points. For the total performance score, add up the weighted points for all the measures.
Why is this important? Each step in the HHVBP calculation is affected by the success of the previous step. If you focus on improving your performance scores, you’re going to end up with higher care points. That leads to higher weighted measure points, which leads to a higher total performance score, which leads to higher percentage of your payment adjustment and, in turn, higher reimbursement and more money for your agency.
Home health is entering a new era
In this new era of care, it’s important for agencies to secure knowledgeable partnerships and adopt digital tools that prioritize meeting CMS guidelines. The result of these relationships can lead to improved HHCAHPS scores and ultimately better total performance scores.
CitusHealth offers technology built for agencies to get secure, real-time communication on any device — driving patient and caregiver satisfaction.
We offer expertise and verbatim commentary to drive better actionable insights — providing in-depth drilldowns of what drives performance and opportunities for improvement.
Connect with us today to learn more about how we can help you meet your needs.
See what MatrixCare can do for you
Liz Silva
With over a decade of valuable experience in the healthcare industry, Liz is a seasoned professional who specializes in working closely with home health and hospice organizations. Her expertise lies in determining strategic needs and seamlessly integrating and utilizing data for informed decision-making. Liz’s proficiency in product management enables her to design user-friendly and quality-driven solutions that empower clients to analyze and comprehend results effortlessly.
Related Posts



See MatrixCare in action
Start by having a call with one of our experts to see our platform in action.
MatrixCare offers industry-leading software solutions. Thousands of facility-based and home-based care organizations trust us to help them improve efficiency and provide exceptional care.
© 2025 MatrixCare is a registered trademark of MatrixCare. All rights reserved.